New Quality Data Requirements
Most hospices keep the majority of their patients comfortable throughout their journey.
However, CMS replaced the HIS with new requirements for quality data to ensure that every patient suffering from a moderate to severe symptom receives timely relief.
Effective October 1, 2025, hospices must submit the Hospice Outcomes and Patient Evaluation (HOPE) data set to CMS. Facilities who fail to submit at least 90% of the required HOPE data will be subject to a 4% payment reduction.
At Admission and two additional in-person visits, nurses must assess and report the severity of 8 key symptoms for each patient.*
If a symptom’s impact is rated as moderate or severe at any of the three HOPE visits, then the hospice must conduct an in-person symptom follow-up visit (SFV) within two calendar days.
*Hope Update Visit (HUV) #1 is required between days 6 and 15 of the hospice stay. HUV #2 is required between days 16 and 30.
Hospice Readiness for HOPE: Practical Steps to Take Now
Webinar: Expert Panel on HOPE
We partnered with Confidis Consulting to offer this panel discussion with hospice industry experts in regulatory compliance (Judi Lund Person, MPH, CHC), EHR implementation (Donnette Threats, MA), and clinical operations (Carla Braveman, BSN, RN, M.Ed.).
This 25-minute video features highlights from the webinar in which the panelists address the current state of hospice industry readiness for HOPE. The panelists also discuss essential steps hospices can take now– focusing on clinical process optimization that will allow for a smooth transition when the EMR updates are released.
Ace the HOPE Symptom Assessments
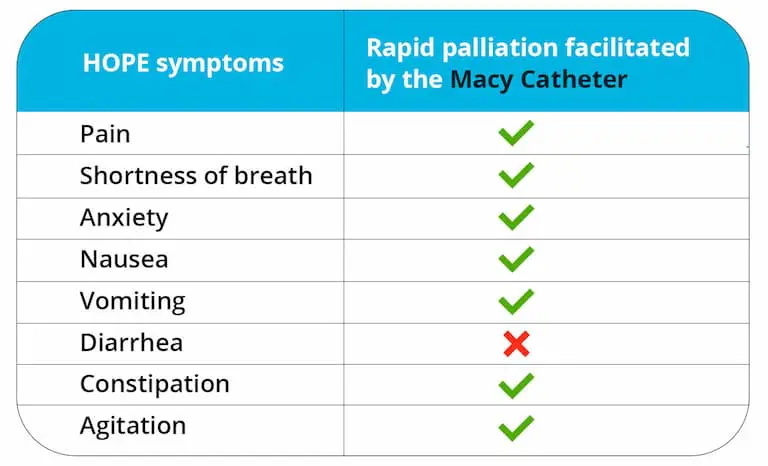
Because the Macy Catheter facilitates quick management of 7 of the 8 HOPE symptoms, hospices can use it to:
Patients report relief 10-15 minutes after receiving medications via the Macy Catheter.
When a nurse finds that a patient’s symptom impact has been moderate or severe during Admission or an HUV, they can use the Macy Catheter to ensure that the visit ends with symptoms under control. The nurse can then immediately conduct the SFV and document accordingly.
Ongoing symptom management is also made easier with the Macy Catheter, because LPNs/LVNs and family caregivers can use it to quickly administer medications (without disturbing the patient). That means fewer SFVs triggered during subsequent HUVs.
Hospices can be confident in their ability to achieve excellent quality metrics without overburdening their staff.

Hospice is CHANGING!
Hospice Nurse Julie’s HOPE Overview
Julie McFadden, RN–known as “Hospice Nurse Julie”–is one of the leading voices working to demystify hospice and end of life care on social media. In this video, she provides a quick overview of the new HOPE data set and explains why it is an important change for hospice.